Dialysis and its Types
What is Dialysis?
Dialysis is a medical procedure used to perform the functions of the kidneys when they are no longer able to effectively filter waste products, excess salts, and fluids from the blood. It is primarily used for individuals with kidney failure or end-stage renal disease (ESRD).
Dialysis helps to regulate electrolytes, maintain proper fluid balance, and remove waste products from the body, essentially performing the crucial functions that healthy kidneys would normally handle. It is a life-saving treatment for those with severe kidney dysfunction or failure.
Why Dialysis is Performed
Kidney Failure: Dialysis is primarily performed in individuals who have experienced kidney failure or end-stage renal disease (ESRD). This condition occurs when the kidneys have lost their ability to filter waste products effectively, leading to a dangerous buildup of toxins in the blood.
Toxin Removal: The kidneys normally filter waste products, excess salts, and fluids from the blood, which are then excreted as urine. In kidney failure, dialysis is necessary to remove these waste products (such as urea and creatinine) from the bloodstream to prevent them from accumulating to harmful levels in the body.
Fluid Balance: Healthy kidneys also regulate the body's fluid balance by adjusting the volume of urine produced. When kidneys fail, dialysis helps to remove excess fluids that can accumulate in the body, leading to swelling (edema) and potentially dangerous fluid overload.
Electrolyte Regulation: Kidneys maintain the balance of electrolytes (such as sodium, potassium, and calcium) in the blood. Dialysis helps to correct imbalances that can occur in kidney failure, preventing complications like hyperkalemia (high potassium levels) or hyponatremia (low sodium levels).
Types of Dialysis
There are two main types of dialysis
- Hemodialysis
- Peritoneal dialysis
Each type has distinct mechanisms, methods, and applications.
1. Hemodialysis
Hemodialysis made up of two words i.e., Hemo meaning "blood" and dialysis meaning "to seperate", so hemodialysis meaning "cleaning of blood".
Hemodialysis involves circulating the patient’s blood outside the body through a dialyzer (artificial kidney). The dialyzer filters out nitrogenous waste products, extra salts, and fluids from the blood.
Procedure
- Blood is taken from the patient’s body through a vascular access (usually an arteriovenous fistula, arteriovenous graft, or central venous catheter).
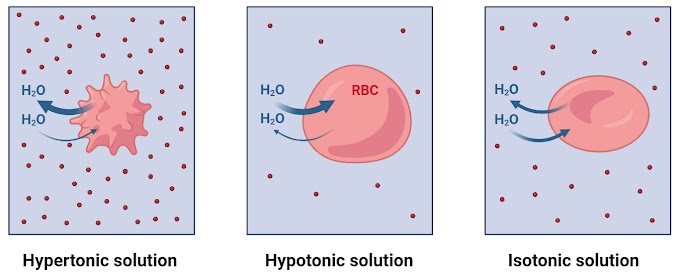
- The blood flows through the dialyzer, where it passes alongside a semipermeable membrane. Dialysis fluid (dialysate) on the other side of the membrane absorbs waste products and excess substances from the blood by diffusion.
- The cleaned blood is then returned to the patient’s body.
Frequency
Hemodialysis is performed three times a week, with each session lasting about 3-5 hours.
Advantages
- Can be done at dialysis centers or at home with appropriate training and equipment.
- Generally more efficient per session compared to peritoneal dialysis.
Disadvantages
- Requires regular visits to a dialysis center (if not done at home).
- Vascular access can be prone to infections and other complications.
- May cause fluctuations in blood pressure and energy levels.
2. Peritoneal Dialysis
In peritoneal dialysis, peri means "around" and teino means "to stretch", altogether it represent the abdominal membrane that is known as peritoneum.
Peritoneal dialysis uses the patient’s peritoneum (the lining of the abdominal cavity) as the filtering membrane. A cleansing fluid called dialysate is introduced into the peritoneal cavity through a catheter, where it absorbs waste products and excess fluids from blood vessels in the peritoneal lining.
Procedure
- A sterile solution (dialysate) is introduced into the peritoneal cavity through a catheter.
- Waste products and excess fluid from the blood pass into the dialysate through the peritoneal membrane.
- After a dwell time (several hours), the used dialysate is drained and replaced with fresh solution.
Types of peritoneal dialysis
1. Continuous Ambulatory Peritoneal Dialysis (CAPD)
The patient manually performs exchanges (draining and filling the peritoneal cavity with dialysate) typically 4-5 times a day.
2. Automated Peritoneal Dialysis (APD)
A machine (cycler) automatically performs multiple exchanges overnight while the patient sleeps.
Advantages
- Can be done at home, offering more flexibility and independence.
- Continuous process that may provide better fluid and waste removal.
- Less dietary restrictions compared to hemodialysis.
Disadvantages
- Risk of peritonitis (infection of the peritoneal cavity).
- Requires patient or caregiver to be trained and capable of performing exchanges.
- Can lead to complications like hernias or peritoneal membrane failure over time.
Importance of Dialysis
Dialysis is a life-saving treatment for individuals with severe kidney dysfunction or failure. Its importance lies in its ability to perform the critical functions normally carried out by healthy kidneys, thus helping to maintain the body's balance and prevent complications associated with kidney failure. Here are the key reasons why dialysis is important:
1. Removal of Waste Products and Toxins
Dialysis helps to remove metabolic waste products such as urea, creatinine, and excess minerals (e.g., potassium and phosphate) from the blood.
Importance
- Accumulation of these waste products can lead to uremia, a condition that causes nausea, fatigue, confusion, and can be life-threatening if not treated.
- By eliminating these toxins, dialysis helps prevent symptoms and complications associated with kidney failure.
2. Regulation of Fluid Balance
Dialysis removes excess fluid from the blood to maintain proper fluid balance.
Importance
- Excess fluid can accumulate in tissues, leading to edema (swelling), hypertension (high blood pressure), and pulmonary edema (fluid in the lungs), which can impair breathing and heart function.
- Proper fluid management through dialysis helps maintain blood pressure and reduces the risk of fluid overload complications.
3. Electrolyte Balance
Dialysis helps to regulate levels of essential electrolytes such as sodium, potassium, calcium, and bicarbonate.
Importance
- Electrolyte imbalances can cause serious issues such as cardiac arrhythmias, muscle weakness, bone disorders, and metabolic acidosis.
- Dialysis corrects these imbalances, ensuring the stability of critical bodily functions.
4. Prevention of Complications
By performing the filtering functions of healthy kidneys, dialysis prevents the buildup of waste and fluid that can lead to severe complications.
Importance
- Preventing complications such as cardiovascular disease, bone disorders, neuropathy, and malnutrition improves the quality of life and increases survival rates for individuals with kidney failure.
5. Support for Other Treatments
Dialysis can be a bridge to kidney transplantation, helping to keep patients healthy enough to undergo transplant surgery.
Importance
- By stabilizing patients' conditions and preventing the progression of complications, dialysis can improve outcomes for those awaiting a kidney transplant.
- Dialysis also supports other medical treatments by ensuring the body can handle medications and therapies that may be required for other conditions.
6. Improvement of Quality of Life
Dialysis allows individuals with kidney failure to continue their daily activities and maintain a more normal lifestyle.
Importance
- While dialysis is time-consuming and requires lifestyle adjustments, it enables patients to live longer and more active lives compared to untreated kidney failure.
- It helps reduce symptoms such as fatigue, itching, and nausea, which are common in advanced kidney disease, thus improving overall well-being.
7. Life Extension
Dialysis sustains life by performing the essential functions of the kidneys in individuals whose kidneys have failed.
Importance
- Without dialysis, patients with end-stage renal disease (ESRD) would face fatal outcomes within a short period due to the buildup of toxins, fluids, and electrolytes.
- Dialysis provides a critical intervention that extends the lives of individuals with kidney failure.
Conclusions
Dialysis is essential for individuals with kidney failure because it replaces the vital functions of the kidneys, removes waste products and excess fluids, regulates electrolyte balance, prevents severe complications, supports other treatments, and improves quality of life. It is a cornerstone therapy that sustains life and helps manage the complex health challenges associated with renal failure.
Both types of dialysis serve the same purpose of removing waste products and excess fluids from the blood but use different methods and have distinct advantages and disadvantages. The choice between hemodialysis and peritoneal dialysis depends on various factors including the patient's medical condition, lifestyle preferences, and the presence of any contraindications to either method. Both types require careful management and coordination with healthcare providers to ensure effective treatment and minimize complications.




0 Comments